In Peques and Más we bring a interview with Dr. Pilar Cots Ivory. She has a degree in Medicine and Surgery from the University of Córdoba and a specialist in Allergology and Clinical Immunology from the Valle Hebrón Hospital in Barcelona. Her experience as a doctor began more than 15 years ago and has worked in different Medical Centers in Barcelona. It is currently the responsible for the allergy consultation of the GEMA Medical Center in Mataró. Pilar combines care practice with a active involvement in the prevention of allergic diseases in schools by conducting periodic workshops and at the level of Health Centers and Hospitals with update sessions on different topics of the specialty. Pilar also belongs to the Spanish Allergy Society (SEAIC), Catalan Allergy Society (SCAIC) and is a partner in the Spanish Association of Parents of Children with Food Allergy (AEPNAA).
Since August 2012 publish your own specific allergy blog in order to contribute their experience and knowledge so that the allergic person and their relatives are able to assume their disease, understand it and live with it in the most natural and balanced way possible. In addition to an allergist, she is the mother of an allergic child, which is a permanent challenge, not only as a mother but also as a doctor. So Pilar is an example to follow because she is very aware of the concerns that any father or mother may have with an allergic child.
Throughout the interview, Pilar will explain to us what parents can do so that the child we expect does not develop an allergy, how to act against a severe allergy, what will happen to the child in school or in his life, when it will improve and many more questions.
Why there are so many cases of allergy in recent years
Currently the allergy is considered as the epidemic of the 21st century in developed countries, so much so that it is expected that by 2025 more than half of the population will be allergic. We all usually know someone who has an allergy or we are the ones who suffer from it. They are generally processes that accompany us for the rest of our life and often influence many aspects of everyday life. All people from birth to death, we are exposed to the environment we have lived, and our health and disease will depend on the ability to respond immunologically.
AdvertisingWe have a surveillance system in our body called the immune system that is what allows everything to work properly, lets the good ones pass and expels the bad ones (viruses, bacteria). When a "wrong" reaction of this defensive system against "things", allergens, with which we are in regular contact (dust, animals, food, etc.) occurs, inflammatory reactions that affect different parts of the body and that we all know as allergy.
And why does this "mistake occur? There is no single cause, probably due to a combination of genetic and environmental factors that, to complicate it further, have to concur at a given time of exposure in the life of each person .
So we have the genetic factors, with which we are born inherited from our parents, and which are divided into several genes making identification difficult. For this reason, children of allergic parents are more likely to have an allergy but not everyone has to be allergic. In addition, we also have to take into account multiple environmental factors, such as exposure to infections, hygiene, contact with animals, pollution, tobacco, food, etc. The western lifestyle leads us to a decrease in infectious processes in the first years of life, this means that our defenses are not activated properly and fail to protect us against the development of allergic diseases. This is the "theory of hygiene", very accepted until a few years ago but now begins to question.
To the enormous responsibility that always has a child, you have to add a significant stress rate if the child also suffers from a chronic illness. The latest data confirm that one in four children (25%) has some type of allergy. The child population is especially susceptible and the symptoms are usually more important. Thus, we can find pictures of atopic dermatitis, chronic respiratory processes (asthma, rhinitis, recurrent bronchitis), otitis, conjunctivitis and severe reactions to dietary staple foods such as milk and eggs. The allergy produces irritability, insomnia and lack of concentration and in case of allergy to a food its intake can produce until the death by an anaphylactic shock. All these diseases entail a significant decrease in the quality of life of the child and his parents.
What differences exist between intolerances and allergies
Allergy necessarily involves an alteration of the immune system. That is, for an adverse reaction to be considered an allergy, it must have an immune basis by force. Currently, doctors have very reliable and rapid tests to diagnose these diseases. This is very important since we usually use the term allergy abusively to explain any reaction to a food.
If there is no alteration of the immune system the reaction can be caused by different causes, from an intoxication (for example by mushrooms) to an intolerance (by an alteration of digestion at the intestinal level, such as in lactose intolerance) but They are not allergic diseases and both their history and their evolution and treatment will be very different.
Avoiding confusion in diseases is important, for example, in food, the only substances capable of producing allergic reactions are proteins. Lactose is a sugar and the inability to digest it correctly is what causes lactose intolerance. This intolerance is not an allergy and can never trigger a severe anaphylaxis as in the case of milk protein allergy. In the case of celiac disease, there is an alteration of the immune system but IgE (immune defense cells) is not involved but other types of cell mediators that trigger a reaction against gluten (protein present in some cereals). For this reason it will not cause serious anaphylaxis, but it is capable of developing other symptoms of general involvement such as skin dermatitis, in addition to digestive. Therefore, celiac disease is not an intolerance (the term gluten intolerance is not appropriate), it is a non-IgE allergy.
Parents who are about to have a baby, what can they do to avoid being allergic
Since we cannot act on the genetic factors involved in allergy, current strategies to prevent these diseases are based on the identification of the environmental factors involved, especially those related to nutrition. It is known that maturation of the immune system takes place from 22 weeks of intrauterine (prenatal) life, until approximately three years of age. During this period the action of different stimuli (food, infections, smoking, etc.) can alter the balance of the defending cells and favor the development of both allergy and other immune diseases (diabetes, psoriasis, ulcerative colitis, etc). To date, numerous studies have been conducted to try to find out if there is any type of diet in pregnancy that may decrease the likelihood of the newborn developing an allergy. For now, the studies are inconclusive, so it is not recommended to "avoid" or "add" any particular food.
During breastfeeding, an allergen-free diet may slightly decrease the possibility of the baby developing atopic dermatitis but would not help prevent the occurrence of other allergic diseases.
The studies support a series of measures during this stage:
- Maintain breastfeeding for a minimum of 4 to 6 months
- If breastfeeding is not possible, it is advisable to administer to children at high risk of allergy (those in which parents are allergic) formulas of hypoallergenic hydrolyzed milk
- Defer the introduction of solid foods to six months. It is not recommended to delay it in excess or stop introducing any food "just in case" since studies show that it can be harmful for proper intestinal digestion. The times must be correct for each food
The realization of food-free diets with high allergenic power (milk, egg, cereals, nuts, fish, etc.) during pregnancy and lactation will NOT prevent the child from developing allergy and also poses a risk due to nutrient deficiency which occurs in the mother and secondarily in the child.
My recommendation is that, in the case of family history of allergy, during pregnancy and the first months of life of the newborn, both the mother and the child make a diet as healthy and balanced as possible and always under the supervision of the specialist involved so that any alteration suggestive of allergy can be detected.
Another important aspect is exposure to tobacco smoke during pregnancy and childhood. It is known to be a risk factor for the baby to develop wheezing (chest pitos) and asthma, especially if the mother is a smoker. In addition, it seems to favor the appearance of new allergies. With respect to allergen exposure, avoidance of dust mites during early childhood can benefit children at high allergic risk (siblings or parents with allergies). As for whether it is advisable or not to avoid pets (dog, cat, rabbit, hamster, etc.), the studies are inconclusive and it is not clear whether or not it could be beneficial, so it is difficult to give a specific recommendation.
No effective strategy has yet been found to prevent the development of allergic disease in children. Probably in the not too distant future and thanks to the studies that are currently underway, we can reach definitive conclusions that help us solve all doubts.
My son is allergic, is there anything I can do to prevent him from having a serious reaction?
When we suspect that our child may be allergic, the first thing we have to do is go to an allergy specialist so he can be diagnosed and treated correctly. In allergic diseases it is essential to perform appropriate preventive measures and thus prevent the reaction from being triggered. The allergist will explain what these measures are depending on the type of allergy your child suffers (dust, animals, plant pollens, food, medicines, latex, insects, etc.) The right information will help you improve your quality of life .
There are two situations that involve an emergency in the life of an allergic child: a severe asthma and anaphylaxis crisis.
Severe asthma crisis occurs in children with respiratory allergies from dust mites, animals, pollens, etc. To try to avoid them, follow some basic instructions:
- Do well the rules and treatment prescribed by the allergist
- Always dispose of the inhaled bronchodilator for urgent use
- Avoid places loaded with smoke (tobacco, chimneys)
- Drinking liquid often so that the airway is hydrated and the mucus can be expelled
- Teach the child to always breathe through the nose as it heats and moistens the air avoiding irritation of the bronchial tubes
- If the child goes to school, they should talk with the teaching staff so that they know how to act and have the medication in case of an asthma crisis. In gym class you should always preheat and avoid running outdoors on very cold days as it is a powerful irritant of the airways. Sport is necessary for the growth of the child and its correct psychomotor and sensory development
The anaphylaxis It is a very serious reaction that involves involvement of different organs of the body. Food is mostly involved in children, although it can also be triggered by allergy to medications, latex and wasp stings, bees. If our child is allergic to a food we must have a series of important precautions:
- Comply with the recommendations prescribed by the doctor and know how and when we should use allergy medication
- The only way to prevent an allergic reaction to a food is by strictly eliminating it from the diet. It should also be borne in mind that reactions can occur by contact, for example, a kiss and by inhalation (fish smoke when cooking, legumes)
- Watch the "grandmother effect" (for a little nothing happens). Food allergy does not influence the amount, with a minimum intake a serious reaction can be triggered
- Be wary of foods labeled "hypoallergenic." Your doctor will give you information about existing alternatives. Always read food labels. Currently, the legislation requires to declare the presence of the most common allergens. Although much progress has been made, there are still many unresolved gaps, among them the definitive elimination of the famous and aided "can contain traces of ...". When in doubt, it is preferable not to consume and call the service phone number available on each product to confirm the ingredients present.
- The situations in which the usual routine is lost are those that carry more risks: parties, excursions, trips, etc. Do not forget to always take the necessary medication for an allergic emergency.
- You should always have your "emergency kit" that contains self-injectable adrenaline (two devices) and syrup antihistamines. It is very important to monitor the expiration of these medications frequently
- Family members and teachers should know the allergy suffered by the child and how emergency medication is administered. Inform the school periodically of any changes in the disease and provide an updated medical report along with the child's personal kit
- In case of allergy to latex or any medication it is convenient to wear a medical alert medal or bracelet
How long can allergy last in children?
Being allergic is an alteration that is not usually modified. But as always, in Medicine, there are exceptions:
- Some children under 4 years old overcome food allergies, although others may develop later. After 4 years the allergy is not usually modified since the immune system is fully formed
- The intensity of the allergy can vary until almost asymptomatic, for example, in children with allergy to a pet, if they stop having contact with her the symptoms disappear. The problem usually reappears if they have frequent contact with the animal over which they were allergic over time.
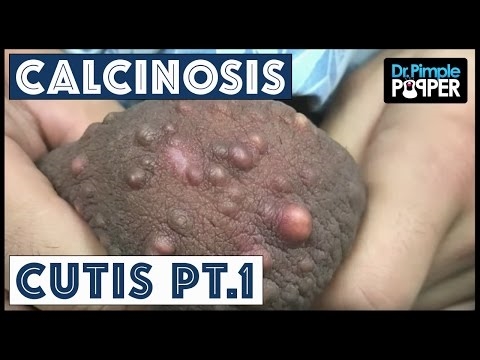
- Atopic dermatitis is an alteration of the immune system that manifests with eczema and itchy skin. The first years of life are the worst but as the child grows the symptoms tend to subside. It is a chronic disease and can reappear throughout different stages of life
"Atopic or allergic gait" is when an allergic involvement of different organs occurs depending on the age of the child. It has been seen that predisposed children often begin within a few months of life with skin symptoms (eczema) or digestive (food allergy) and, over time, after 4 years, give way to a involvement of the bronchi (asthma) and nose and eyes (rhinoconjunctivitis).
Currently, allergists have two types of measures that can help control allergic disease:
- Immunotherapy or allergy shots. This treatment is the only one capable of modifying the course of the allergic disease, either by reducing the symptoms and even healing the patient. The success rate is very high provided the patient is well chosen and the vaccine to be used. This is why it is important that it is a specialist doctor who prescribes it. The problem is that there are currently no previous tests to know how a certain patient will respond to immunotherapy and the only way to know is to try it for a while. It consists of administering to the child the substance to which he is allergic in increasing amounts, so that "tolerance" is induced. So the allergen will stop causing symptoms. It can be used from 4-5 years of age, orally (sublingually) or punctured (subcutaneous). It is used to treat allergic rhinoconjunctivitis, allergic asthma and allergy to bee venom and wasps. WHO has confirmed the efficacy of vaccines in these diseases. So far, its effectiveness in atopic dermatitis is not yet proven and there are no vaccines of this type to cure food allergy, although much research is being done.
- Desensitization or induction of oral tolerance (ITO). Recently applied, this method does not usually start before 5 years of age, to allow time for spontaneous healing to occur. The risk of an inadvertent intake causing a severe anaphylaxis has led to the investigation and implementation of this type of action. It is done by gradually administering increasing amounts of the food involved (milk or egg) so that the child can eventually tolerate a certain amount and thus avoid serious reactions with minimal intakes of the food to which he is allergic. It is very important that once the goal is reached, the child takes the stipulated amount of milk or egg that he has been able to tolerate daily, in this way the immune system does not forget what has been learned. Spain is one of the pioneer countries where this induction of oral tolerance is being carried out successfully in children very allergic to these foods. Progress over the next few years will be very important.
Both immunotherapy and ITO are always performed following the allergist's instructions, with strict medical control to detect and treat any adverse reactions. Both represent a certain hope towards healing.
How allergic children feel with their surroundings
Despite being in contact with many of them in the office and having my child allergic to multiple foods, getting in their skin is not easy. We already know that children are like sponges and that their ability to adapt is usually amazing, it could not be less in the case of allergy. Thus, as a general rule, the child lives this situation without dramatisms or complexes and usually engages this fact in his daily life with an admirable naturalness.
It is evident that this is not always the case, that there are many associated variables and that each child will live them differently according to each space and time in their day to day. One of the most important variables is the age at which the allergy appears. A child who becomes allergic with a few months of life is not the same as the one who develops the allergy at 8 years. The personal and family way of living that problem will not be the same.
An allergic young child, with less than four years, has that allergy in his life. Thanks to the efforts of the parents, that child acquires dietary habits in which the foods that give him allergy are out of his daily routine and he will assume it, in principle, naturally.
When the allergy appears in an older child, their attitude is usually different. Suddenly, a child who ate something regularly and without problems, becomes allergic and has to stop eating, with what he liked! That child, of course, will initially live that prohibition in his life as something negative, he will remember the things "so rich" that he can no longer eat and that his friends can, although generally they eventually adapt and assume it without problems. They become true "detectives" and are able to thoroughly read all labels with their ingredients. Nor do they eat anything until they are totally sure that they do not carry their "allergic food." These children have experienced an allergic reaction and their memory is the best help against forgetting. They represent a great example for allergic adults who are less receptive to change.
From the age of 12, the child enters adolescence and this stage is especially delicate for food allergy sufferers. They are old to be responsible for their disease and this means a "dose of burden" that many refuse to assume. They stop being careful, do not carry the medication and are able to play their lives by making a grace in front of friends. It is the age at which the danger of anaphylactic shock is greater. It is a stage in which neither doctors nor parents can relax. You have to remind them from the responsibility the importance of life itself.
The childhood of an allergic child does not have to be different from that of others. Your allergy cannot and should not be a limitation in your personal and social development. My experience shows me every day that these children mature quickly, assume their problem naturally and, what is even more striking, they are usually the ones who help their parents to live the allergy as something "normal" in their life. They are examples of improvement for all.
How can we inform parents about the questions we have about allergies?
25% of children suffer from some type of allergy, 15% are asthmatic and almost 10% are allergic to any food. The figures indicate the increasing frequency of this disease in developed countries. Being a chronic problem makes us accompany the rest of our life, for this reason it is very important to have all the necessary information, in a clear and updated way.
The main and most important thing is to have an allergist who we trust 100%, to whom we can ask all the doubts and, above all, to easily access any important problem. Communication is essential for parents with an allergic child to feel safe.
In addition, in the times in which we live, we cannot forget access to information through the Internet and social networks. Although it is true that its indiscriminate use without filters usually involves a "headache" for the doctor before the patient "poorly informed." It is no less true that if they are used in a balanced way, accessing reliable and valid sources, it is a very valuable tool that can greatly facilitate the relationship between the doctor and the patient.
The allergy content that we can find on the Internet is very varied and not all recommended. My advice is always that you inform yourself in the pages of medical societies such as the Spanish Society of Pediatric Allergy (SEICAP), in patient associations and in blogs with medical accreditation. Since the end of last year, with little time but with much enthusiasm, I decided to get involved in the task of disseminating health knowledge through social networks and I launched a blog where you can access many pages of resources of interest about allergies in a way Safe, fast and reliable.
To end the interview, Pilar, to whom We appreciate your generosity in the answers with such detailed content, wants to leave us a reflection that, she says we should try not to forget the parents that we have allergic children although I think we all have to know:
The allergic child is a healthy child, without symptoms, unless he comes into contact with what gives him allergy. As any child will play, study, celebrate the birthday of friends and go on an excursion with the immense illusion that always accompanies this magical stage of life